Legionella – A Deadly Healthcare Acquired Infection
Each year 4 in 100 hospital patients acquire an infection related directly to their hospital stay, known as a Hospital/Healthcare-Acquired Infection (HAI). These HAIs may be caused by any number of pathogens; viral, fungal or bacterial. One of the most fatal of HAIs is an infection caused by Legionella, namely Legionnaires’ Disease, which is found in water. It is estimated that 33% of HAIs are from water, which is why a comprehensive water management plan is critical to keep patients safe.
Legionella bacteria form, grow and thrive in favorable water system conditions that include the presence of stagnant water, biofilm formation, good food sources, sufficient oxygen in the water and optimal water temperatures. Optimal water temperatures for Legionella growth are the same temperatures found in most hospital hot water loops. Bacteria multiply best in temperatures between 77-108 deg C and optimally thrive a 95 deg F.
 Online CDC Legionella Risk Assessment
Online CDC Legionella Risk Assessment
One of the biggest concerns in a health care environment is that the warm water can be aerosolized, such as in water cooling towers, showers and water fountains. Other potable water functions in a health care environment where warm water temperatures may lead to Legionella bacteria formation include water used for sanitation, heating, ventilation, air conditioning, laundry, food services, ice production, bathing, physiotherapy, pools, cleaning medical devices and lab procedures. Also, decorative environmental water features such as waterfalls and fountains may have water temperatures optimal for the formation, growth, and transmission of Legionella bacteria. Patient exposure to Legionella bacteria-contaminated water may lead to Legionnaires’ Disease.
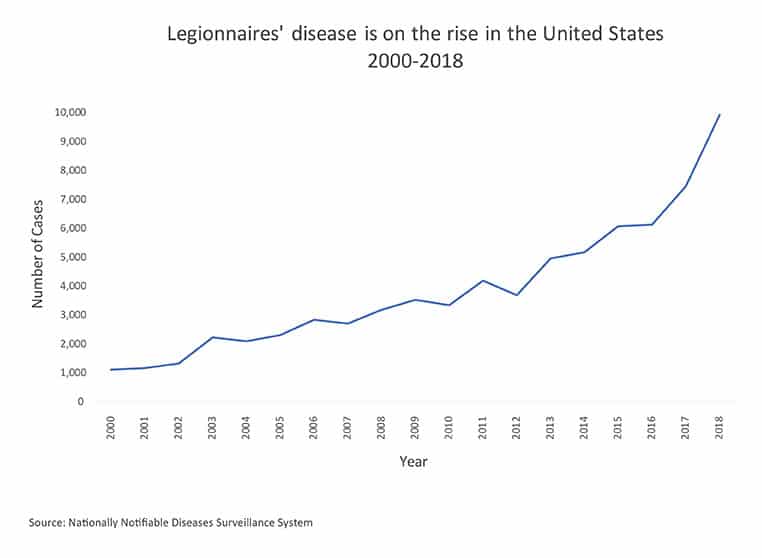
In 2015, the Center for Disease Control (CDC) studied the occurrence of healthcare-associated cases of Legionnaires’ Disease. This research found that it was impossible to determine a definite number of Legionnaires’ Disease cases attributable to health care due to the extensive number of ways a patient may have been exposed to contaminated water. It is estimated that 90% of cases do not get identified. The vast majority of patients who contract pneumonia are not tested for Legionnaires’ Disease. This lack of testing is the root cause that true number of Legionnaires’ Disease cases is much higher than reported. However, it was found that every metropolitan area included in the study did have reported cases of Legionnaires’ Disease that were health care-associated and the fatality rates were staggering.
Twenty-five percent (25%) of the definite healthcare-associated cases of Legionnaires’ Disease were fatal. In another ten percent (10%) of the fatal Legionnaire’s Disease cases, there was strong possibility that the contracted Legionnaires’ Disease was healthcare-associated. In other words, 1 in 4 persons with definite healthcare-associated Legionnaires’ Disease died.
This high fatality rate of healthcare-associated Legionnaires’ Disease sheds light on the importance of case prevention activities including the implementation of effective water management programs.
“Prevention and response require coordination amount health care facility leaders, health care providers, and public health professionals. Instituting and maintaining effective water management programs are the principal prevention measure.” – Center for Disease Control (CDC)
Contact Legionella Control Systems for a Legionella risk assessment and Legionella testing.







